UK’s first gene therapy baby celebrates 21st birthday
The first child to be treated in the UK with gene therapy celebrated his 21st birthday last week, twenty years after having the pioneering treatment at Great Ormond Street Hospital for Children (GOSH).
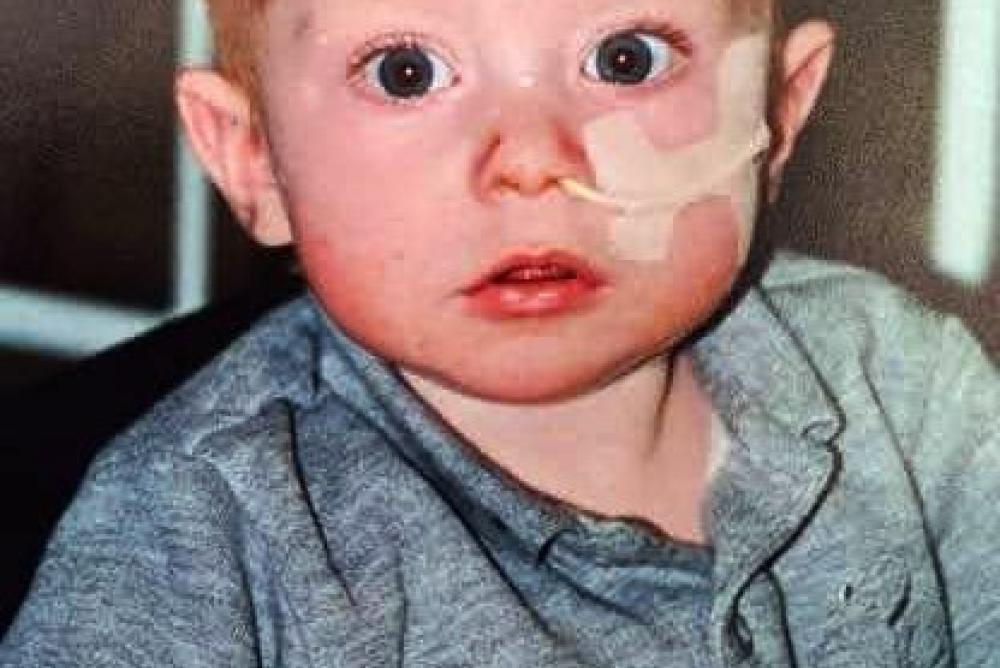
Dubbed ‘bubble boy’ by many, Rhys Evans from Cardiff was born with a rare disease, Severe Combined Immunodeficiency (SCID), that left him vulnerable to even the most minor infection. Rhys was just a year old when his parents made the brave decision for him to be the first child in the UK to receive the therapy. He's now a healthy young adult heading off to university.
Since that historic moment at GOSH, over 100 children have been treated with gene therapy for dozens of different diseases. Many of these children would have been expected to die before their second birthday and gene therapy has been transformational in allowing many of them to live normal lives and go to school.
Gene therapy was pioneered at GOSH by Professor Bobby Gaspar and Professor Adrian Thrasher who were working on a revolutionary new type of therapy where a working copy of the gene could be inserted into the patients’ own cells using a modified, harmless virus. Much of this early research took place at the Wolfson Centre for Gene Therapy, supported by the Wolfson Foundation.
Back in 2001, the only treatment for patients like Rhys was a bone marrow transplant, an incredibly difficult procedure. Rhys became the first to receive this ground-breaking gene therapy and after a few weeks his immune system started to develop.
The majority of patients treated in clinical trials at GOSH with gene therapy have had different forms of SCID, but more recently patients with a range of diseases from leukaemia to rare genetic conditions such as Spinal Muscular Atrophy and an inherited retinal disorder which causes children to lose their sight - Lever’s Congenital Amaurosis – have been treated in clinical trials. GOSH is now a global centre of excellence for gene therapy and has treated more patients with the technology than anyone else in Europe.
Among those leading the clinical trials are Professor Claire Booth – who recently celebrated the successful results of a stem cell gene therapy clinical trial for ADA-SCID - and Professor Manju Kurian, who discovered the brain disorder dopamine transporter deficiency syndrome (DTDS) in 2009 and has subsequently helped develop a potential gene therapy cure for the disease. Both Professor Claire Booth and Professor Manju Kurian’s work is supported by GOSH Charity.
For example:
- Most clinical trials of gene therapy involve an ‘infusion’ or injection of the treatment, targeting conditions that can be treated in the blood stream (leukaemia and SCIDs) but research into direct treatment of the brain and the eye are well underway, opening the door for hundreds of rare conditions, affecting thousands of children.
- Wiskott-Aldrich syndrome - a rare genetic immune disorder - has already been treated at GOSH using gene therapy on stem cells from bone marrow but scientists are now investigating if CRISPR-Cas9, the ‘molecular scissors’, can do this more effectively and efficiently.
- Clinical trials at GOSH for leukaemia have already used CRISPR-Cas9 technology to ‘programme’ T-cells to recognise and target cancer cells. This CAR T-cell research is ongoing to see if it can be used to target other cancers in children with no other hope for treatment. Next steps will see if so-called ‘base-editing’ can be used to fix the genes themselves, without cutting the cells’ DNA.
This is a true celebration of research changing lives and we are incredibly proud of what our research teams and clinicians have been able to achieve over the last two decades. It takes huge teams to bring treatments out of the earliest stages of development in the lab and into patients and we can only hope that this continues and we’re able to do more and more with this technology to help more patients.
Mat Shaw, CEO of GOSH
Jinhua Xu-Bayford is a Gene Therapy and Immunology Clinical Nurse Specialist lead at GOSH and has been involved in the gene therapy programme from the very beginning: “I used to work on the immunology and Bone marrow transplant wards and looked after children with SCID for whom conventional treatment was not always a viable option. . When we started being able to offer gene therapy for patients as alternative, it was so wonderful to be able to tell parents that there was another chance for their child that could transform their life.
“I have more or less personally infused every single gene therapy patient in a trial here and have seen the technology evolve into something that has a hugely positive impact on so many lives. Clinical trials are a massive piece of teamwork, and it is a tremendous effort to bring in patients – many from across Europe – to receive life-saving treatment. We know we simply have to do all we can to help and I am very proud to be a part of this.”
Much of the pioneering gene therapy research at GOSH takes place in the purpose-built Zayed Centre for Research into Rare Disease in Children. The Centre brings together state-of-the-art research and clinical care under one roof and is a partnership between GOSH, GOSH Charity and University College London. The Centre was made possible by a £60m gift from Her Highness Sheikha Fatima bint Mubarak, wife of the late Sheikh Zayed bin Sultan Al Nahyan, Founder of the United Arab Emirates, continued support from the Wolfson Foundation and funding from Great Ormond Street Hospital Children’s Charity.


