Facial Palsy
概述
Great Ormond Street Hospital has a long history of caring for children and young people with facial palsy, including those with Moebius. Professor Grobbelaar led the service for the last decade. He was trained at Mount Vernon by Mr Douglas Harrison, who first described the two-stage procedure for facial reanimation with the pectoralis minor in 1983. Mr Woollard was, in turn, trained by Professor Grobbelaar. He has been running the service for adults at the Royal Free Hospital for the last ten years, and now leads the Great Ormond Street service as well since Prof Grobbelaar retired last year. This has linked up the paediatric and adult facial palsy care and established a strong link for patients to ‘graduate’ through as they grow too old for GOSH. Facial palsy is a condition that needs life-long care and this ensures that patients get continuity.
Most patients are referred to the service soon after birth when a difference in facial expression is noticed. At this visit we can assess the child and give information to the parents. Provided there is no need for urgent treatment (typically for eye protection) and the baby is able to feed and thrive we will next see them at around two years of age to start the discussion about possible interventions.
At four, when it is becoming easier for children to demonstrate a fuller range of expression, it it is possible discuss surgery in more detail and make a plan for the coming years (see below).
Our Approach

Mr. Alexander Woollard
Our service is led by Consultant Plastic Surgeon Mr Woollard, lead for the facial palsy service at Great Ormond Street.
Unilateral Facial Palsy: Two-Stage Surgery
The mainstay of this approach in children is a two-stage operation in unilateral facial palsy. This involves a cross-facial nerve graft at around the age of 4–5 years. This is where a sensory nerve is taken from the lower leg (sural) and used to bridge the gap from the nerves on the functioning side across to the paralysed side, akin to an extension cable.
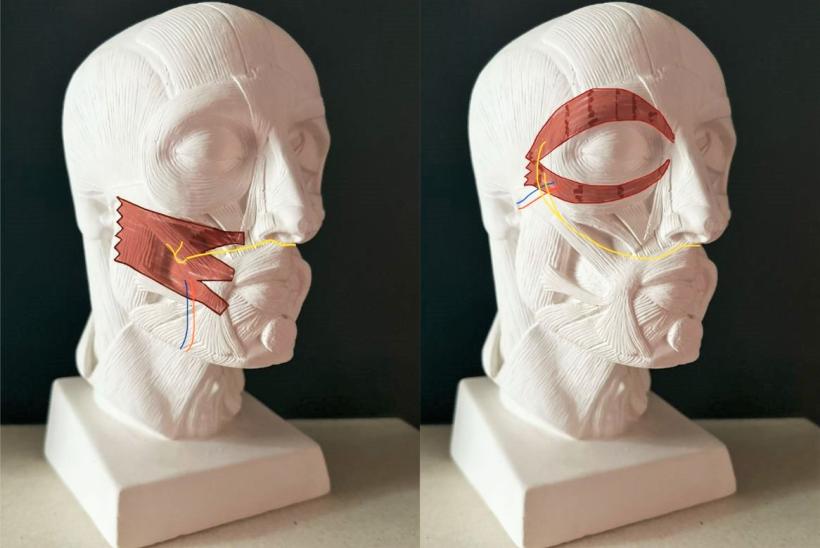
The typical facial nerve has five main branches: the forehead, the eye, the upper lip, the lower lip and the neck. Those branches all have multiple smaller branches, and the one to the eye and the upper lip also have lots of crossover, which means it is possible to ‘borrow’ one. On the functioning side, a small branch that makes the upper lip smile is used as the input and the graft run across under the nose to the other ear. The nerve fibres gradually grow along the graft and in 6–12 months reach the other side.
Muscle Transfer and Nerve Connection
At that point, at a second operation, a muscle is taken from the armpit (typically the pectoralis minor) and placed in the paralysed cheek. It needs a blood supply to keep it alive and healthy, and the nerve graft is connected to the nerve that makes it twitch. It doesn’t work straight away, but the nerve makes new connections with the muscle and in 3–6 months it starts to contract. At that point, physiotherapy begins with specialist exercises to help gain control over the movement and optimise the surgical outcome.
Bilateral Facial Palsy and Moebius Syndrome
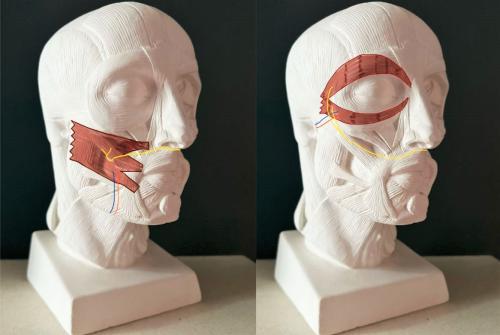
In Moebius, it is more complicated. There isn’t a facial nerve on either side, so there is no option for a nerve graft. In bilateral facial palsy, we need to find an alternative source for the nerve to make the muscle move. In most cases, this can be the nerve in one of the biting muscles in the cheek (the masseter).
Bilateral Muscle Transfer Using the Masseter Nerve
A muscle is taken from each armpit (the latissimus dorsi), and once placed in each cheek, attached to the facial blood vessels and wired up to a branch of the nerve to masseter. This means that, once the nerve has made a new connection, biting will elicit movement from both cheeks, emulating a smile.
We aim to do this between 8 and 16 years of age because, in children, they are more able to learn to use that smile with emotion, even though it is powered by biting. It isn’t the same as connecting it to the ‘smiling nerve’ on the other side as we do in unilateral facial palsy, but because it is bilateral and symmetrical, it provides expression.
At GOSH we prefer to transfer both muscles in a single surgery.

Our specialist staff
We have a strong multi-disciplinary team at Great Ormond Street, from the experienced staff on Panther ward to specialist anaesthetist, physiotherapist and plastic surgery clinical nurse specialists. We hope that this summary will help prospective patients to better understand the team and what we can offer.
转诊您的孩子前来治疗
如您想转诊您的孩子,请填写下方的转诊申请表。我们的同事会在2个工作日内与您取得联系。
必填项