Research funded by GOSH Charity has the potential to transform the lives of children with epilepsy
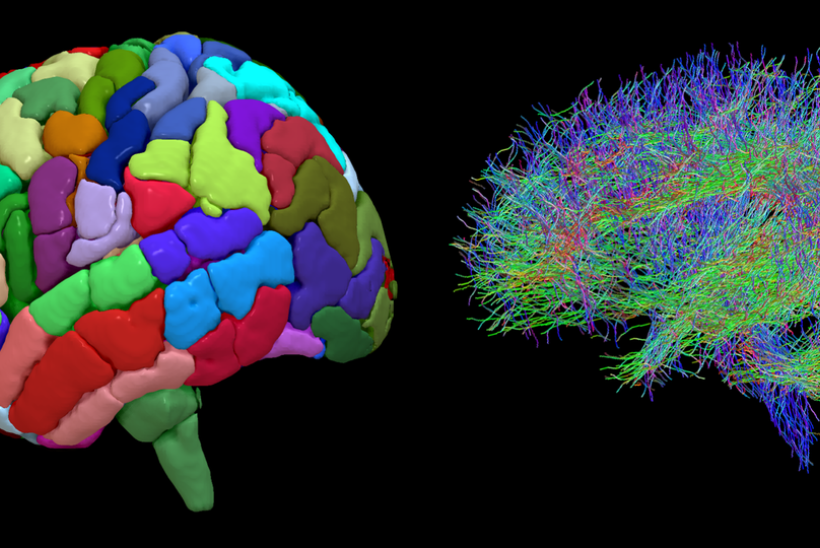
Structural imagine of the brain’s regions (left) and diffusion diagram of the wiring of a brain (right), which Lewis-Spitz Surgical Scientist Aswin Chari and his team analyse together to create a ’network’.
The brains of children with epilepsy are wired differently to those without the condition, a new study found.
Researchers at Great Ormond Street Hospital (GOSH) and UCL Great Ormond Street Institute of Child Health (UCL GOS ICH) have been working to understand more about epilepsy in children.
Their findings pave the way for improved surgical treatment of the condition.
A closer look at the findings
Lewis-Spitz Surgical Scientist Aswin Chari, whose role is funded by GOSH Charity, led the team carrying out the research.

The team used a technique called diffusion MRI to analyse wiring diagrams of the brain. This enabled them to see how strongly different areas of the brain are connected to each other.
Children with epilepsy had differently wired brains. They had more connections than children without epilepsy.
It is thought that these unusual wiring dynamics make them more likely to have epileptic seizures.
Children whose seizures stemmed from multiple areas of the brain had greater differences in wiring than those with seizures stemming from only one area.
Of the 79 children with epilepsy who were part of the study, 52 had surgery to remove the brain regions responsible for their seizures.
The brain areas removed were found to have particularly more abnormal wiring than other brain regions. Removing them led to more normal wiring dynamics in the brain.
Whilst not all participants were cured of their seizures, the research team hopes that the technology and analysis used in this study will pave the way for further studies – leading to improved surgical outcomes and more children being offered the procedure.
Mr Chari said: “I am delighted to share the findings of this study, in which we used diffusion MRI technology to teach us about the function of children’s brains, helping to deepen our understanding of debilitating conditions like epilepsy.
“Although surgery for epilepsy is relatively safe, it is a large undertaking and there are some children who undergo surgery but sadly continue to have seizures. We hope through this technology and analysis, we can enable more children with the condition to benefit from life-changing surgery and treatment.”
Meet GOSH Nurse Millie
Millie is a nurse on GOSH's Koala Ward and is responsible for looking after children with epilepsy.
Millie also has her own experience of epilepsy. She was diagnosed with tuberous sclerosis complex when she was a baby – a rare genetic condition that causes epileptic seizures.
In 2020, when she was 26, she had surgery to remove part of her left temporal lobe and her hippocampus, the parts of the brain found to be causing her seizures. Her operation was a success and Millie is now seizure free and enjoying the new freedom this brings.

“I was diagnosed with tuberous sclerosis complex when I was a baby after having my first seizure. Back then I was having tonic-clonic seizures. Medication stopped those seizures, but I then started having two to three focal seizures a week – these are a bit less angry.
“Epilepsy has always been a big part of my life. As well as having the condition myself, I work on GOSH’s Koala ward, which is a neurosurgical ward, and I’ve always done charity work linked to epilepsy. I was probably very naïve as to how much epilepsy affected me.
“As a child no one ever gave my parents the option of surgery, but in adulthood, because of my job as a nurse and my interest in epilepsy, I found that I may be eligible for surgery. I eventually had the surgery in July 2020 when I was 26 years old.
“When I stopped having seizures post-surgery, I felt like I’d lost a bit of my identity. I almost had to remind myself I still have the condition. It’s like someone who brushes their teeth twice a day being told they no longer need to brush their teeth. I remember saying to my husband, “What do normal people think about?”.
While life post-surgery has been a big adjustment for Millie, she reflects on the change she’s seen in her mental wellbeing. “My mental wellbeing and energy levels have massively improved. I will now go for really long walks, sometimes for two or three hours. Two years ago I wouldn’t have even gone to a supermarket on my own when I was feeling unwell. There’s a lot more freedom to my life that I didn’t realise I was missing beforehand.
“It would be amazing if the new research conducted by Mr Chari and his team means more children are given the option to have the surgery when they’re younger. As children’s brains are still growing they can recover more quickly than an adult brain following treatment. I've been on antiepileptic drugs for so long, that I will never fully come off them. If surgery had been an option when I was younger, I could have stopped the medication and my brain would have grown to not need it.”
A collaborative effort
The research was a collaborative effort between GOSH, UCL GOS ICH, King’s College London, The University of Pennsylvania and Nemours Children’s Hospital. It was underpinned by support from the GOSH National Institute of Health Research Biomedical Research Centre.
It comes almost a year after the Royal College of Paediatrics and Child Health (RCPCH) revealed in the Epilepsy 12 report that three quarters (77%) of children who should have been considered for epilepsy surgery in November 2020 had not been referred. It also identified issues around waiting times for tests, treatment and referrals to paediatric neurologists.
While these figures can be partly attributed to the COVID-19 pandemic’s impact on healthcare, Mr Chari and his team hope their findings will mean more children can be diagnosed and treated more effectively and efficiently.
Thank you to GOSH Charity supporters
GOSH Charity’s Director of Impact and Clinical Programmes at Great Ormond Street Hospital Children’s Charity., Dr Kiki Syrad, thanked GOSH Charity supporters for helping to make research like this possible.
“We at GOSH Charity are proud to have funded this important study which has the potential of transforming the lives of children with epilepsy and other brain conditions," she said. "It is thanks to the generosity of our supporters that GOSH Charity can continue to fund life-changing research which benefits seriously ill children from across the UK.”