Technology is changing the way paediatric medical care is delivered
The healthcare industry is rapidly evolving. Technologies that a few years ago seemed a figurative idea of the future, are now being utilised to improve patient well-being, reduce pain and even save lives. Innovation in the context of paediatric surgery is leading to more precise and less invasive interventions for children, and today, healthcare professionals can leverage innovative technologies to treat complex cases to address the needs of children suffering from disease or disabilities.
Mr. Greg James, Consultant Neurosurgeon, and Mr. Martin Tisdall, Consultant Paediatric Neurosurgeon who are part of the Neurosurgery Team at Great Ormond Street Hospital for Children (GOSH) in London look at how innovation has transformed the practice of neurosurgery to deliver more effective and precise treatment for children.
Innovations in neurosurgery
ETV-CPC
Hydrocephalus is a condition where the patient has a build-up of fluid in the brain, and results in an abnormal widening of spaces in the brain. One to two of every 1,000 babies are born with hydrocephalus, which makes it as common as Down’s syndrome and more common than spina bifida or brain tumors[1].
ETV-CPC is a revolutionary technique, which reduces the risk of fluid production in the brain, and often means less follow-ups for patients compared to the traditional brain shunt procedure. The procedure, now available to patients treated at GOSH, offers international patients the chance to have a better quality of life and limits the life-long burden of care, which often comes with having the traditional shunt procedure.
Mr. Greg James explains that there are no medical therapies available to treat hydrocephalus and the only options are surgical[2]. “The traditional way to treat hydrocephalus is with a shunt. While it is still a very good operation that is conducted commonly, it leaves the patient with a permanent tube in the body to allow for the draining of the fluid. The limitations with any tube or mechanical device is that it can snap, it can get blocked, it can get infected and cause problems. ETV-CPC gives the patient the chance to avoid the lifelong burden of care that comes with having a shunt,” Mr. James added.
“The procedure is well-tolerated and only takes an hour or two. The child can then go home within a day or two of the operation,” he says.
Gamma Knife
Gamma knife is a very precise and well-established form of radiotherapy. During the procedure, doctors can determine which areas will get radiation and which areas will not, in order to limit the brain’s exposure to radiation. Mr. James says, “Gamma Knife works like a colander. It uses very weak beams which then all intersect and generate a high dose of radiation. Meanwhile, the surrounding brain area is protected and limited to a very low dose of radiation”.
The procedure is set to improve the lives of hundreds of children suffering from arteriovenous malformations (AVMs). This technique offers potentially lower risks to the patient compared to other surgical options currently available and offers a long-term solution for deep and small AVMs that are impossible to operate on using traditional approaches.
“Published evidence indicates that there is an 80-85% complete cure of AVMs with Gamma Knife,” says Mr. James. He also stresses that the procedure is extremely safe and the child should be able to go home the next day. “Generally we do the treatment on a Friday and the kids are back at school on a Monday. So they tolerate it very well,” he says.
Endoscopic suturectomy
For the 1 in 2500[3] children who suffer from craniosynostosis, which is when the early closure of sutures of the skull which causes an abnormally shaped head, endoscopic suturectomy offers a less invasive solution.
Mr. James explains “the skull is not one big bone, it is made of different plates. Sometimes, babies can be born with one or two of these sutures fused, which is called craniosynostosis. This causes the abnormal growth of the skull and causes problems with pressure within the skull and also with the brain.”
In order to treat craniosynostosis, surgical intervention is needed. Traditionally this would be done with a large operation that would leave a large scar and require removing pieces of bone to remodel the skull. “These traditional operations,” Mr. James explains, “take many hours and involve a week, or sometimes longer, stay at hospital with the potential need for blood transfusions. The new operation, endoscopic suturectomy, offers a less invasive option for families.”
Endoscopic suturectomy is a small keyhole procedure which removes a small piece of bone and takes less than an hour. After the operation, children are fitted with a specially made helmet which encourages the skull to grow through pressure. “The published results are very positive and suggests that due to the ability to do the operation at a very young age, it is also improving associated facial deformities and so improve squints and other ocular problems.”
Epilepsy
More than 720,000 people with epilepsy live in the Arab world.[4] “Epilepsy is the most common chronic neurological problem,” Mr. Tisdall explains “It can be caused by many different things; anything that damages the brain.”
The majority of affected children are able to have their epilepsy controlled by medicine, but about quarter of children do not respond to medicine. “When a patient has drug-resistant epilepsy, after the first few drugs tried have failed, the chances of them being seizure-free with medication alone drops to around 5%. With surgery, we can offer a 65-70% chance for these selected patients to become seizure free.”
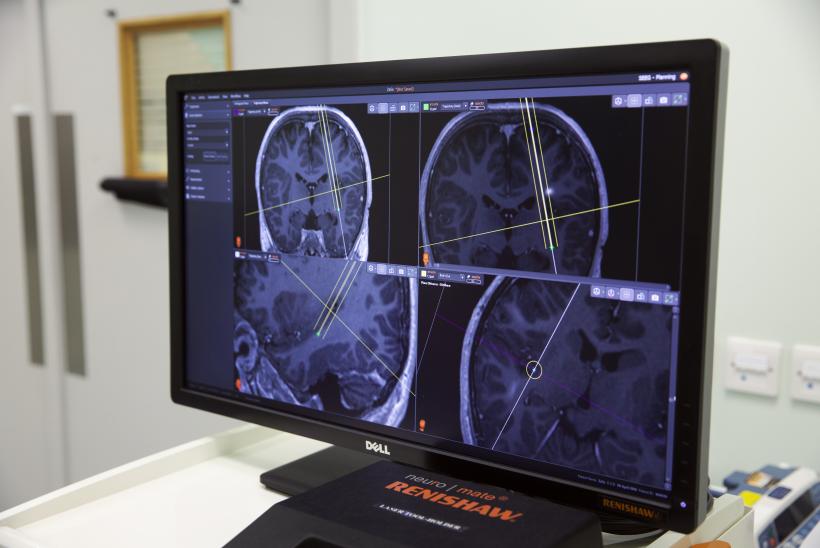
In order to make epilepsy surgery more accurate and safer for the patients, Mr. Tisdall and his team began a programme to use Stereoelectroencephalography (SEEG) to map the electrical signals in the brain.
SEEG allows recording from deep in the brain as well as the base of the brain and inner surfaces in a less invasive manner. “With SEEG we place very fine wires into the brain in multiple areas. These wires are placed through tiny incisions and little bolts, which reduces the risk of infection, and children tolerate it much better than the open surgery alternative. It involves a quicker recovery and only a very small procedure is required to remove the wires.” The procedure is less invasive when compared to traditional subdural grid, which required making a large window in the skull and placing a mat of electrodes over the surface of the brain.
To increase the accuracy of placing the SEEG electrodes, a stereotactic robot is used. “It’s a system for guiding the wires into the brain in a very accurate way so that we can improve safety by avoiding blood vessels and increasing accuracy.”
Mr. Tisdall and his team are constantly looking for ways to improve the accuracy and safety of their operations. “We are increasingly moving towards using computerised 3D models of the brain to help us improve our ability to understand where we are in the brain.”
The neurosurgery department at GOSH provides a tertiary service for children with disorders of the brain and spine that require surgical management. It offers surgical opinions, investigations and treatments for severe and complex patients through a multi-disciplinary team.
[1] Facts and stats. Hydrocephalus Association. Available at: http://www.hydroassoc.org/about-us/newsroom/facts-and-stats-2/
[2] Facts and stats. Hydrocephalus Association. Available at: http://www.hydroassoc.org/about-us/newsroom/facts-and-stats-2/